Cervical Lymph Nodes in CA Prostate: An Easiest Tool to Deal with Diagnostic Dilemma
Pankaj Srivastava, Shalini Srivastava and Sunil Kumar
DOI10.21767/2576-3903.100028
Pankaj Srivastava1*, Shalini Srivastava1 and Sunil Kumar2
1Department of Surgery, Om Surgical Center and Maternity Home, Varanasi, Uttar Pradesh, India
2Department of Oncology, Om Surgical Center and Maternity Home, Varanasi, Uttar Pradesh, India
- *Corresponding Author:
- Dr. Pankaj Srivastava
Laparoscopic, Thoracic, Thoracoscopic & VATS Surgeon
Department of Surgery, Om Surgical Center
and Maternity Home, Varanasi, Uttar Pradesh, India
Tel: +91-542-2586191
E-mail: drpankajbns@gmail.com
Received Date: March 28, 2018 Accepted Date: April 07, 2018 Published Date: April 11, 2018
Citation: Srivastava P, Srivastava S, Kumar S (2018) Cervical Lymph Nodes in CA Prostate: An Easiest Tool to Deal with Diagnostic Dilemma. J Neoplasm Vol.3: No.1: 3. doi: 10.21767/2576-3903.100028
Abstract
Cervical lymphadepathy is very common in many benign and malignant conditions. It is not only the easiest accessible tissues for making the correct diagnosis by histopathologic examination (HPE) but also may be the only presenting feature of the disease. We herein present a case of prostate cancer that was diagnosed only by the HPE and Immunohistochemistry (IHC) of the excised cervical lymph nodes. The importance of cervical lymph node biopsy has also been discussed.
Keywords
Cervical; Lymph node; Prostate; Prostate cancer; Malignancy; Lymph node biopsy; Immunohistochemistry
Abbreviations
HPE: Histopathologic Examination; FNAC: Fine Needle Aspiration Cytology; IHC: Immunohistochemistry; PSA: Prostate Specific Antigen; PSMA: Prostate-Specific Membrane Antigen
Introduction
Prostate cancer may present as wide spectrum of disease from asymptomatic to distant metastasis with systemic involvement. The axial skeleton, retroperitoneal lymph nodes and the regional lymph nodes are the most frequent sites of metastasis but distant metastasis to the left supraclavicular nodes is rare presentation. Although cervical lymph nodes are a common site of metastasis for head and neck malignancies, metastasis from the prostate is extremely rare [1]. Few authors have presented their reports of prostate cancer with cervical lymphadenopathy as an initial presentation of the disease [2-6].
Case Presentation
A 61-years-old smoker, non-alcoholic, non-vegetarian male, truck-driver by profession presented with pain in passing urine with mild to moderate pain in lumbar and pelvic region which slowly progressed to right lower limb. There was no history of fever, hematuria, burning micturition, pain in abdomen and trauma. Patient had no significant past medical and family history. There was no history suggestive of diabetes mellitus, hypertension, tuberculosis and any chronic viral illness. On examination, multiple enlarged lymph nodes were found in the anterior triangle along with mass in the left supraclavicular region measuring approximately 3.5 x 3.0 cm. The lymph nodes were nontender, firm to hard in consistency with restricted mobility over the deeper structures. Skin over the swelling appeared normal. There was no bruit. Physical examination of the abdomen and pelvis was unremarkable. The external genitalia, scrotum and testes were also unremarkable. Patient refused for the digital rectal examination (DRE) and even for trans-rectal ultrasonography (TRUS). Ultrasonography of the abdomen revealed bilateral hydronephrosis with multiple enlarged retroperitoneal lymph nodes causing pressure over the ureters. Prostate was enlarged to volume of 24 mL but no focal lesion detected. Liver and other intra-abdominal organs were unremarkable. There was no evidence of ascitis. These findings were confirmed by CECT abdomen and pelvis. Other systemic examinations were normal. The biochemistry and serology tests were normal but serum prostate specific antigen (PSA) was 178 ng/mL. Since the patient had not given consent for trans-rectal prostatic biopsy, we decided to go for excisional biopsy of cervical lymph nodes preferably the supraclavicular node to have an idea of primary lesion.
After proper consent, excisional biopsy of supraclavicular node was taken under local anesthesia. Wound closed by 4/0 prolene sutures and dressed properly. Patient’s recovery was uneventful. Stitches were removed after day 7 with no complication.
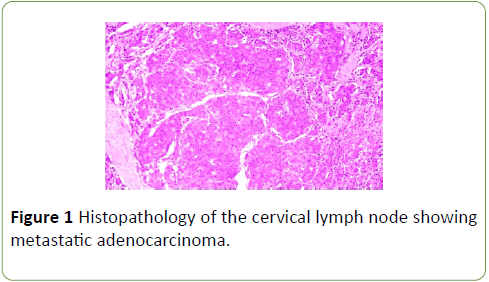
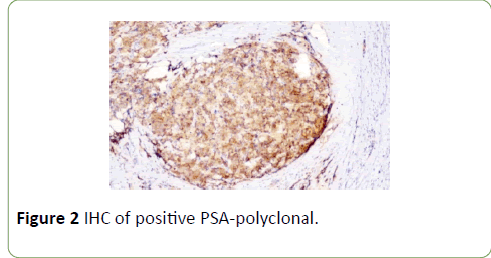
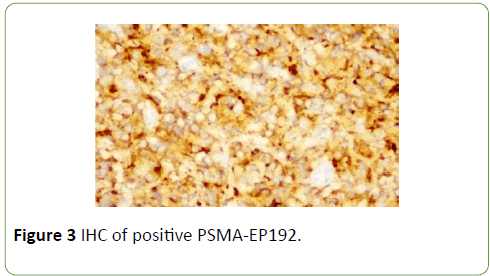
Gross examination of the excised left cervical lymph node was a tan-yellow to tan-white nodular soft tissue piece measuring 2.0 x 1.0 x 0.8 cm. External surface was nodular. Cut section was tan-white and hemorrhagic. Histologic examination revealed metastatic adenocarcinoma. The tumor cells were arranged in glands, sheets, cords, and focally forming cribriform spaces. Individual tumor cells were monomorphic with prominent nucleoli (Figure 1). PSA Polyclonal (Figure 2) and Prostate-specific membrane antigen, PSMA-EP192 (Figure 3) both were positive. Final diagnosis of the metastatic adenocarcinoma of the prostate was made.
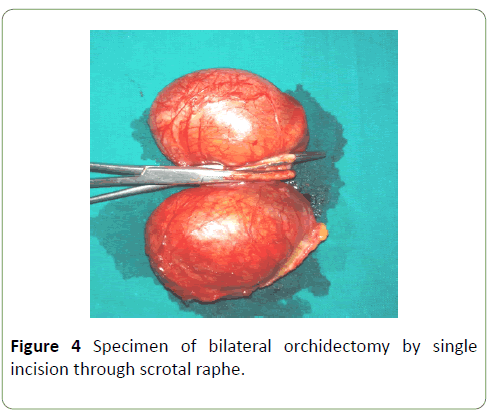
Patient was started with the bicalutamide and leuprolide but subsequently also underwent bilateral orchidectomy (Figure 4) as an anti-androgenic therapy. Serum PSA level came down to 2.7 ng/mL after three months of treatment. For lumbar and pelvic bone pain, zoledronic acid 4 mg in 100 mL of 0.9% sodium chloride was also given. Patient responded well with the therapy and stable till one year of our follow-up without any evidence of recurrence. Bilateral hydronephrosis was resolved as retroperitoneal lymph nodes regressed markedly after treatment.
Discussion
Prostate cancer may present itself in many ways staring from the most common voiding symptoms to the rare metastatic cervical lymphadenopathy. Cervical lymph nodes may get enlarged in many benign and malignant lesions from the local surrounding structures but distant metastasis to these lymph nodes from remote areas are not common. The common sites for metastasis of prostate cancer include bone, regional lymph nodes, lungs, bladder, liver and adrenals. The most common spread of prostate cancer is via direct invasion to the pelvic organs or vertebral bodies [4].
Regarding distant metastasis, Dutta et al. [7] demonstrated that tumor cells and tumor-derived growth factors, cytokines and other molecules can enter into the lymphatic tracts through the hyper-permeable lymphatic endothelial cells. They subsequently traffic to the regional lymph nodes, distant lymph nodes and finally to the blood circulation, where they can metastasize to distant organs. Therefore, tumor-associated lymphatic vessels form an easy passage of tumor cells to lymph nodes and distant organs.
Wang et al. suggested that the current assessment of cervical lymphadenopathy presumed to be metastatic in nature involved careful history taking and physical examination and after FNAC if doubt remained about the origin of the tumor, lymph node biopsy with specific IHC must be undertaken [6].
We did the same as above since the patient refused for the DRE and even for the TRUS guided prostatic biopsy, thus cervical biopsy made the final diagnosis. Though the tissue biopsy cleared the diagnosis of metastatic adenocarcinoma, use of specific IHC with PSA and PSMA helped a lot for further confirmation of prostate as primary. Bernacki et al. suggested that IHC for PSMA was more sensitive than that for PSA in the cytodiagnostic workup of metastatic prostate cancers. Of note, the combination of PSMA and PSA immunohistochemistry was slightly more sensitive than the sensitivity of utilizing PSMA immunohistochemistry alone [8]. Thus it indicates that if anyhow excisional biopsy of cervical lymph nodes is not available, one may make diagnosis with FNAC and further IHC with the cell-blocks.
Treatment with bicalutamide, leuprolide combined with orchidectomy suffices to allay the symptoms and maintain the quality of life. The role of radiation is limited to palliation of local symptoms related to neural compression or venous obstruction [4].
Conclusion
Though the initial presenting features may not be related to the cervical lymphadenopathy but if these nodes are enlarged and palpable, excisional biopsy of these lymph nodes may give valuable information of the primary lesion. IHC may further be helpful in evaluation of the type of tumor. Prostate cancer should also be included in the differential diagnosis of cervical lymphadenopathy or cervical mass lesions irrespective of the serum PSA levels and presence or absence of other associated symptoms. High index of suspicion is required to find out the origin of the metastasis. Treatment of metastatic adenocarcinoma of prostate with bicalutamide, leuprolide and bilateral orchidectomy still stays effective.
References
- Hematpour K, Bennett CJ, Rogers D, Head CS (2006) Supraclavicular lymph node: Incidence of unsuspected metastatic prostate cancer. Eur Arch Otorhinolaryngol 263: 872-874.
- Elabbady A, Fouad-Kotb AF (2013) Unusual presentations of prostate cancer: A review and case reports. Arab J Urol 11: 48–53.
- Lin YY, Lin DS, Kang BH, Lin YS (2011) Neck mass as the first presentation of metastatic prostatic adenocarcinoma. J Chinese Med Asso 74: 570-573.
- Dubhashi SP, Kumar H, Nath SR (2012) Prostate cancer presenting as cervical lymphadenopathy. Am J Case Rep 13: 206-208.
- Chan G, Domes T (2013) Supraclavicular lymphadenopathy as the initial presentation of metastatic prostate cancer: A case report and review of literature. Can Urol Assoc J 7: e433-e435.
- Wang HJ, Chiang PH, Peng JP, Yu TJ (2004) Presentation of prostate carcinoma with cervical lymphadenopathy: A report of three cases. Chang Gung Med J 27: 840-844.
- Datta K, Muders M, Zhang H, Tindall DJ (2010) Mechanism of lymph node metastasis in prostate cancer. Future Oncol 6: 823–836.
- Bernacki KD, Fields KL, Roh MH (2014) The utility of PSMA and PSA immunohistochemistry in the cytologic diagnosis of metastatic prostate carcinoma. Diagn Cytopathol 42: 570-575.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences