FDG-PET/CT-Positive Foreign Body Granuloma Mimicking Colon Cancer Recurrence: Case Report
Germano de Sousa Leão, Gabriele Taumaturgo Mororó, Andressa Marques Campelo de Carvalho, Sávia Raquel Costa Normando, Sabas Carlos Vieira and Danilo da Fonseca Reis Silva
DOI10.21767/2576-3903.100024
Germano de Sousa Leão*, Gabriele Taumaturgo Mororó, Andressa Marques Campelo de Carvalho,Sávia Raquel Costa Normando, Sabas Carlos Vieira and Danilo da Fonseca Reis Silva
Gastroenterology Institute, Universidade Federal do Piaui, Brazil
- *Corresponding Author:
- Germano de Sousa Leão
Gastroenterology Institute, Universidade
Federal do Piaui, Brazil
Tel: +55 (86) 99810-9968
E-mail: germanoleao18@gmail.com
Received Date: December 06, 2017 Accepted Date: December 24, 2017 Published Date: December 30, 2017
Citation: De Sousa Leão G, Mororó GT, De Carvalho AMC, Normando SRC, Vieira SC (2017) FDG-PET/CT-Positive Foreign Body Granuloma Mimicking Colon Cancer Recurrence: Case Report. J Neoplasm. Vol.2 No.3: 15.doi: 10.21767/2576-3903.100024
Abstract
Colorectal cancer (CRC) is the third most prevalent malignancy worldwide, and one of the most common causes of cancer-related deaths. The main tumor-related prognostic factor after surgical resection is initial pathologic staging and lymph node involvement is a major determinant of disease recurrence. The addition of adjuvant chemotherapy in stage III patients undergoing surgical resection decreases tumor recurrence by around 40% to 50%. However, a significant proportion of patients still experience systemic recurrence. In CRC, 18F-FDGfluorodeoxyglucose (18F-FDG-PET-CT) plays a key role in the detection of recurrent disease in post-therapy assessment of residual masses and patient staging before surgical resection of liver metastases. We report the case of a 52-year-old patient with stage III colorectal cancer, who underwent surgical resection and completed adjuvant chemotherapy, followed by imaging techniques (Fluorine-18-FDG PET-CT and magnetic resonance) mimicking early peritoneal and ovarian recurrence.
Keywords
Colorectal cancer; 18F-FDG PET-CT; Recurrence; Mimicking
Introduction
Colorectal cancer (CRC) is the third most prevalent malignancy worldwide, and one of the most common causes of cancer-related deaths [1,2]. Surgical resection of the primary tumor associated with 6 months of adjuvant chemotherapy is standard treatment in patients with stage III CRC. Nevertheless, even after treatment, systemic recurrence in particular is frequent and may affect half of these stage 3 patients [3].
Therefore, intensive patient follow-up is crucial for early detection of metastases and possible therapeutic interventions that may increase overall survival [4]. Follow-up includes ultrasonography and computed tomography (CT). Fluorine-18-FDG PET-CT scan has demonstrated a higher accuracy for the detection of malignant lesions in comparison to other methods, particularly in the context of CRC [5]. We present a case of a 52-year-old patient diagnosed with stage III adenocarcinoma of the colon. Early ovarian and peritoneal lesions emerged after the completion of adjuvant chemotherapy, which mimicked recurrence of CRC shown by Doppler pelvic ultrasonography and confirmed by MRI and 18F-FDG PET-CT.
Case Presentation
A 52-year-old female patient developed acute abdominal obstruction and underwent exploratory laparotomy, which revealed a left colon tumor. A left hemicolectomy with primary anastomosis associated with regional lymphadenectomy was performed. Histopathology study (HP) revealed a welldifferentiated adenocarcinoma, with subserosal tissue invasion and metastasis in one out of sixteen resected lymph nodes. The tumor was classified as Stage IIIb (pT3pN1).
In the postoperative period (PO), she progressed with fecal peritonitis, and was re-operated with the construction of a colostomy. Early tumor staging with CT scans (CT) of the chest and abdomen did not detect any significant alterations, except for a left hypodense adnexal lesion, measuring 2 cm. The mass had a cystic aspect and was probably of ovarian origin. Transvaginal ultrasound revealed a predominantly cystic heterogenous formation, with well-defined margins and absent flow on Doppler, in addition to normal Ca-125 level. After clinical improvement, she initiated adjuvant chemotherapy using 12 cycles of 5-fluorouracil, leucovorin and oxaliplatin, at a total duration of 6 months.
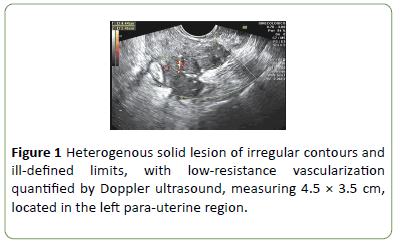
After the completion of adjuvant therapy, new follow-up CT scans revealed enhancement of left axial lesion and the emergence of a hypodense collection in the left lower parietocolic gutter, measuring 2.9 cm × 1.5 cm. Transvaginal ultrasound indicated the presence of a septated cystic lesion with coarse septae in the right adnexal region measuring 4.6 × 4.4 × 2.8 cm. This mass was associated with a solid lowresistance vascularized lesion in the left adnexal region, measuring 4.4 × 3.4 cm (Figure 1).
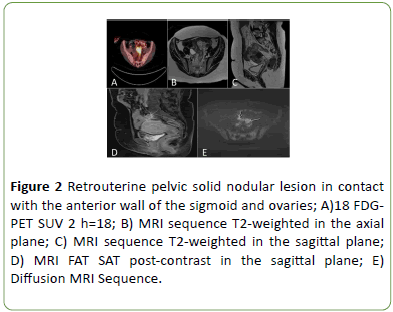
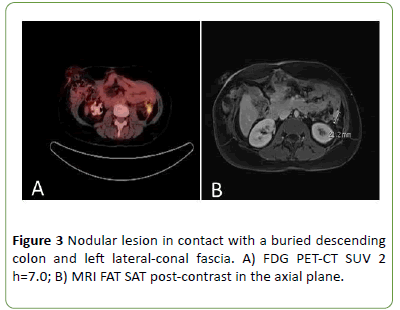
A 18F-FDG PET-CT showed increased radiopharmaceutical uptake in expansive pelvic lesion with signs of infiltration in both ovaries and intimate contact with the wall of the sigmoid and uterine fundus (SUVMAX of 18.1) (Figure 2A-2E), associated with increased uptake in peritoneal thickening along the margin of surgical resection adjacent to the left colon (SUVMAX 7) (Figure 3A). Magnetic resonance imaging (MRI) corroborated previous radiologic findings, indicating the presence of solid nodes in contact with a buried descending colon (Figure 3B), retrouterine space in contact with the anterior wall of the sigmoid and ovaries, and the left anterior pararenal fascia compatible with secondary implants (Figures 2B-2E).
Figure 2: Retrouterine pelvic solid nodular lesion in contact with the anterior wall of the sigmoid and ovaries; A)18 FDGPET SUV 2 h=18; B) MRI sequence T2-weighted in the axial plane; C) MRI sequence T2-weighted in the sagittal plane; D) MRI FAT SAT post-contrast in the sagittal plane; E) Diffusion MRI Sequence.
A reoperation was indicated. Surgical planning involved cytoreductive surgery and hyperthermic intra-peritoneal chemotherapy (HIPEC) if the disease was restricted to the peritoneum and if complete cytoreduction was accomplished. The patient chose to forgo HIPEC, and only opted for cytoreductive surgery. In the intra-operative period, there were nodes of malignant aspect in the pelvis, lateral peritoneum and ovaries. A bilateral oophorectomy associated with node resection was performed, with sigmoid resection and protective ileostomy. The patient developed bowel obstruction and peritoneal infection in the postoperative period, requiring a new operation. She remained hospitalized for 30 days.
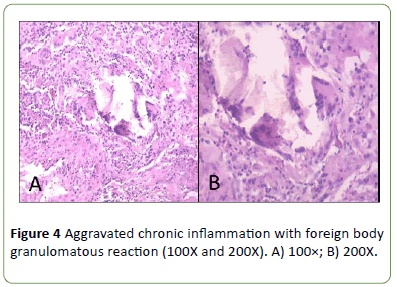
Histopathology study revealed no malignancy, presence of adnexal epithelial inclusion cysts and aggravated chronic inflammation with foreign body granulomatous reaction (Figures 4A and 4B). The patient is clinically well, showing no evidence of disease recurrence after 18 months since surgery and the ileostomy was closed.
Discussion
Patients with CRC and regional node involvement are a heterogenous subgroup since patients are grouped with different grades of primary tumor invasion (any T) associated with lymph node involvement (N1 and N2). The median fiveyear survival rate may range from 44% to 84% [6,7]. Clinically non-detected micrometastases may exist, increasing the risk of tumor recurrence. Nevertheless, this risk decreases by about 40% to 50% in stage III patients who receive adjuvant chemotherapy. However, in 35% of cases there is still the possibility of recurrence, systemic in particular [8]. The ovaries are among the least involved metastatic sites and are affected in less than 5% of patients [2,9,10]. In the current report, after ending adjuvant therapy, the patient exhibited alterations in imaging studies suggestive of ovarian involvement of malignant origin.
In women with a suspicion of adnexal lesions, both Doppler ultrasound and magnetic resonance imaging are sensitive methods for identification of malignant lesions. However, the specificity of MRI is significantly higher [11,12]. On follow-up of CRC, 18F-FDG PET-CT plays a fundamental role in the detection of recurrent disease, in the evaluation of posttherapy residual masses and in patient staging before surgical resection of liver metastases. This diagnostic method has a sensitivity and specificity of 88% and 94%, respectively, on evaluation of disease recurrence in CRC [13]. Furthermore, the test has a positive predictive value of 96.4% and negative predictive value of 76.9% [14].
In the current report, after the completion of adjuvant therapy, follow-up CT scans revealed bilateral adnexal masses. On assessment by transvaginal Doppler ultrasonography, these masses were vascularized. Vascularization indexes assessed by Doppler 3D are significantly higher in malignancies, revealing vascularity that increases in central regions to the detriment of peripheral regions [15]. On MRI, solid peritoneal nodes were compatible with secondary implants. Fluorine 18-FDG PET scan showed increased radiopharmaceutical uptake in the expansive pelvic lesion with signs of infiltration in both ovaries and intimate contact with the wall of the sigmoid and uterine fundus (SUVMAX of 18.1) corroborating the diagnostic hypothesis of tumor recurrence after combined analysis of imaging test results.
However, after bilateral oophorectomy, histopathology study of specimens revealed that the masses were composed of fibrous scar tissue, possibly related to repeat surgical approach for management of fecal peritonitis. Surgical materials and instruments may cause inflammatory reactions and foreign body giant cells. Depending on the nature and extent of the reaction produced, lesions such as intraabdominal adhesions and tumor masses may be induced, mimicking metastasis in oncologic cases [16].
Limitations of 18F-FDG PET-CT include false-positive results, generally occurring in cases of acute or chronic inflammation, lymphadenitis, nonspecific reactions after radiation therapy, abscesses and foreign body granulomatous reactions. All these processes may demonstrate increased uptake, since they may have a high rate of glucose metabolism. These conditions can mimick malignant tumors and thus reduce precision of the test. To increase specificity of the test, levels of laboratory markers, such as carcinoembryogenic antigen (CEA) are correlated. In the presence of elevated CEA levels, the test has positive predictive values of 89% and negative predictive values of 100% [17,18].
Another alternative to distinguish malignant lesions from benign inflammatory processes is "Dual Time point PET". Dual time point PET is a technique where image acquisition is performed after a standard uptake phase and then repeated after a delay. This technique has been studied by many investigators and can be a useful method in differentiation between benign and malignant causes of FDG accumulation in PET scans.
There are other cases in the literature describing lesions suspected of tumor recurrence in CRC by PET-CT scan, which proved to be benign only after histopathology study (Table 1) [14,17-24].
| Gender | Age (years) | Stage | Interval PO | Location |
|---|---|---|---|---|
| F | 69 | II | 5 years | Lesion located at the left side of the abdominal aorta. |
| F | 61 | IV | 10 months | Lesion located in the left hypochondrium in area below the ligament of Treitz |
| F | 39 | II | 16 months | Lesion in the mesentery in peripancreatic area. |
| F | 31 | II | 7 months | Multiple lesions located along the hepatic surface, in parietal peritoneum adjacent to segment 3 and posterior to the surface of segment 6 of the liver. |
| F | 48 | IV | 1 year | Lesion in margin of segment 7 of the liver. |
| M | 55 | II | 5 years | Lesion located in surgical scar at midline of the abdomen |
| M | 38 | II | 3 years | Lesion located in the cecum. |
| F | 47 | II | 7 weeks | Lesion located in right paracolic area. |
| M | 64 | III | 7 weeks | Lesion located in pelvic region proximal to the right iliac vein. |
| M | 71 | IV | 4 months | Lesion located in stump of liver resection. |
| F | 59 | IV | 7 years | Lesion located in the left posterior side of the larynx. |
| M* | 65 | - | - | Peritoneal lesions with splenic invasion. |
* Article in Japanese
Table 1: Cases in the literature with false-positive PET-CT in CRC.
Conclusion
Follow-up of patients with adenocarcinoma of the colon may be challenging. Understanding the biologic behavior of CRC, associated with follow-up complementary tests, always bearing in mind that a false-positive result may occur is essential for the correct diagnosis and choice of the most adequate therapy.
Conflict of Interest
The authors declare no conflicts of interest.
Author contributions
DFRS is the advisor. SRCN is the co-advisor. DFRS proposed the study of the case report. GTM, GSL and AMCC researched and wrote the first draft. DFRS collected and along with SRCN analyzed data. All authors contributed to the creation and interpretation of the study.
Acknowledgements
We thank the patient ZMAAL for allowing us to expose her case in the study; the UDI imaging clinic for granting us the images, digitized transvaginal ultrasound, along with image description; and Sírio-Libanês Hospital for granting us the resonance images of the lower abdomen.
References
- Ye Y (2015) Pre-operative TNM staging of primary colorectal cancer by 18F-FDG ET-CT or PET: A meta-analysis including 2283 patients. Int J Clin Exp Med 8: 21773-21785.
- Baratti D (2016) Progress in treatments for colorectal cancer peritoneal metastases during the years 2010-2015. A systematic review. Crit Reviews Oncol/Hematol 100: 209-222.
- Riechelmann R, Grothey A (2017) Antiangiogenic therapy for refractory colorectal cancer: current options and future strategies. Ther Adv Med Oncol 9: 106-126.
- Compton C (2002) Pathologic prognostic factors in the recurrence of rectal cancer. Clin Colorectal Cancer 2: 149-160.
- Gao G (2013) Meta-analysis of the additional value of integrated 18FDG PETeCT for tumor distant metastasis staging: Comparison with 18FDG PET alone and CT alone. Surg Oncol 22: 1-6.
- Silva T (2013) O índice de linfonodos comprometidos como um preditor para a ocorrência de recidivas tumorais no câncer de cólon estádio III. Rev Col Bras Cir 40: 463-470.
- Greene F (2002) A new TNM staging strategy for node-positive (Stage III) colon cancer. Ann Surg 236: 416-421.
- André T (2009) Improved overall survival with oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment in stage II or III colon cancer in the MOSAIC trial. J Clin Oncol 27: 3109-3116.
- Kobayashi H (2007) Characteristics of recurrence and surveillance tools after curative resection for colorectal cancer: A multicenter study. Surgery 141: 67-75.
- Omranipour R (2009) Ovarian metastases in colorectal cancer. Int J Gynecol Cancer 19: 1524-1528.
- Veena RI, Susanna IL (2010) MRI, CT, and PET/CT for ovarian cancer detection and adnexal lesion characterization. AJR Am J Roentgenol 194: 311-321.
- Guerriero S (2010) Transvaginal color doppler imaging in the detection of ovarian cancer in a large study population. Int J Gynecol Cancer 20: 781-786.
- Almuhaideb A, Papathanasiou N, Bomanji J (2011) 18F-FDG PET/CT Imaging. Oncology Ann Saudi Med 31: 3-13.
- Orii T (2015) An FDG-PET/CT-positive lesion mimicking local recurrence of colon cancer 5 years after radical colectomy. Am J Case Rep 16: 149-152.
- Lima JC (2010) Diseases malignas ovarianas: importância atual da ultrassonografia no rastreamento e manejo e manejo terapêutico. Femina 38: 257-260.
- Tripathi PB, Kini S, Amarapurkar AD (2009) Foreign body giant cell reaction mimicking recurrence of colon cancer. Trop Gastroenterol 30: 219-220.
- Lim JW, Tang CL, Keng GH (2005) False positive F-18 fluorodeoxyglucose combined PET/CT scans from suture granuloma and chronic inflammation: report of two cases and review of literature. Ann Acad Med Singapore 34: 457-460.
- Matsuura S (2016) Silk suture granuloma with false-positive findings on PET/CT accompanied by peritoneal metastasis after colon cancer surgery Int J Surg Case Rep 28: 22-25.
- Pantiora EV (2016) Granuloma mimicking local recurrence on PET/CT after liver resection of colorectal liver metastasis: A case report. Cureus 8: e717.
- Audollent R (2015) Pitfalls and mimickers on (18) F-FDG-PET/CT in peritoneal carcinomatosis from colorectal cancer: An analysis from 37 patients. J Visc Surg 152: 285-291.
- Bajin MD, Hosal AS (2013) A false-positive FDG uptake in Teflon granuloma: A case report. Ear Nose Throat J 92: E1-2.
- Crucitti A (2013) Food residue granuloma mimicking metastatic disease on FDG-PET/CT Jpn J Radiol 31: 349-351.
- Mori Y (2014) False-positive local recurrences on FDG-PET/CT due to postoperative infection: a case report. Gan To Kagaku Ryoho 41: 1599-1601.
- Basu S (2011) Fundamentals of PET and PET/CT imaging. Ann N Y Acad Sci 1228: 1-18.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences