Anaemia in Cancer Patients Undergoing Radiotherapy and Chemotherapy at the National Hospital, Abuja
Aruah SC, Oyesegun R, Ogbe Oche, Jawa Z, Itanyi U, Ugwuanyi CU, Aniwada EC, Ezikeanyi SI, Odume B, Amadi P, Okwor V and Ige T
DOI10.21767/2576-3903.100012
Aruah SC1*, Oyesegun R1, Ogbe Oche2, Jawa Z3, Itanyi U4, Ugwuanyi CU5, Aniwada EC6, Ezikeanyi SI7, Odume B8, Amadi P9, Okwor V10 and Ige T11
1Department of Radiation Oncology, National Hospital Abuja, PMB 425, Garki Abuja, Nigeria
2Department of Haematology, National Hospital Abuja, Nigeria
3Department of Nuclear Medicine, National Hospital Abuja, Nigeria
4University of Abuja Teaching Hospital, Nigeria
5Department of Neuro Surgery, National Hospital Abuja, Nigeria
6Department of Community Medicine, University of Nigeria College of Medicine, Enugu, Nigeria
7United Nations Population Fund, Abuja Office, Nigeria
8U.S Centers for Disease Control and Prevention (CDC) Abuja, Nigeria
9Federal Medical Centre, Abuja, Nigeria
10Department of Radiation Oncology, University of Nigeria Teaching Hospital, Enugu, Nigeria
11Department of Medical Physics, National Hospital Abuja, Nigeria
- *Corresponding Author:
- Chinedu Simeon Aruah
Department of Radiation Oncology
National Hospital Abuja
PMB 425, Garki Abuja, Nigeria
Tel: +2348037419877
E-mail: aruasimeonedu@yahoo.com
Received Date: May 30, 2017; Accepted Date: June 26, 2017; Published Date: July 04, 2017
Citation: Aruah SC, Oyesegun R, Ogbe O, et al. Anaemia in Cancer Patients Undergoing Radiotherapy and Chemotherapy at the National Hospital, Abuja. Ann Clin Lab Res. 2017, 2:2. doi: 10.21767/2576-903.100012
Abstract
Anaemia is one of the predisposing factors to poor patient outcome in cancer treatment. More than 50% of cancer patients will receive either Radiotherapy or Chemotherapy or both in the course of their treatment. It has been difficult to establish global or National benchmark on the baseline haemoglobin of patients selected for cancer therapy at different stages of the tumours. Various centers use different levels but there is a need to establish a national cut-off point. Establishing a uniform benchmark will inform a global best practice and increase the patient’s outcome and quality of life. The acceptable value of anaemia varies from centre to centre but Hb level of 10 g/dL in both male and female are usually acceptable in most Radiation Oncology Centers in Nigerian Hospitals. Haemoglobin level of 10 g/dL is a borderline value and administration of Radiotherapy or Chemotherapeutic agents however without adequate hematological support may tilt the patient into clinical anaemia. This prospective study was done to determine the pattern of anaemia in cancer patients undergoing Radiotherapy and Chemotherapy in Nigeria using 201 cancer patients enrolled in National Hospital Abuja with histopathologically confirmed malignancies (solid cancers). The prevalence of anaemia in the study was 63%. The impact of Chemotherapy on Hb level was more significant than in other treatment arms, hence Chemotherapy – 9.60-10.62 g/dL, Radiotherapy 11.52-12.13 g/dL, and Chemoradiation 10.98-11.36 g/dL. The HB level continually decreased in all arms of treatment. We recommend a benchmark of 11 g/dL minimum for any patient being selected for Radiotherapy, Chemotherapy and Chemoradiation in Nigeria.
Keywords
Anaemia; Cancer; Haemoglobin; Radiotherapy; Chemotherapy; Chemoradiation
Introduction
Many cancer patients present with anaemia prior to Radiotherapy and Chemotherapy and most even experience anaemia or worsening of anaemia at some point during treatment. The acceptable value of anaemia vary from centre to centre but a Hb level of 10 g/dL in both male and female are usually acceptable in most Radiation Oncology Centres in Nigerian Hospital for therapeutic purposes. Haemoglobin level of 10 g/dL is a borderline value and administration of Radiotherapy or chemotherapeutic agents however without adequate haematological support may tilt the patient into clinical anaemia. The pathophysiology of cancer-related anaemia have been studied and found to be multifactorial [1].
The pathophysiology of cancer-related anaemia have been studied and found to be multifactorial [1]. Anaemia usually occurs as a consequence of direct inhibitory effect of inflammatory cytokines, erytbropoietin deficiency, blunted erythropoietin response, blood loss, nutritional deficiencies, renal insufficiency, socio-cultural and religious factors. Also treatment-associated factors may aggravate the incidence of anaemia and these may compromise patient’s tolerance of treatment [4]. Generally, patients with low haemoglobin have a reduced loco-regional tumour control and survival probability. While several mechanisms can be proposed to explain this relationship, tumour hypoxia is clearly one of the major factors. Although a well-documented causal relationship between Hb concentration level, tumour oxygenation and response to radiotherapy and chemotherapy have not been shown, it is nevertheless likely that such a relationship do exist and there is thus rationale for investigating the possibility of improving treatment outcome in cancer patients undergoing radiotherapy and chemotherapy in radiation oncology department.
Several studies have shown that tumours are more hypoxic than the surrounding normal tissue [5]. Tumour cells can become resistant to cancer treatment because of hypoxia; this is due to decrease oxygen transport capacity as a result of tumour associated anaemia. Hypoxic regions have been identified by Nordsmark et al. in locally and advances breast and cervical cancer, head and neck cancers, rectal cancer, brain tumours, soft tissue sarcomas and malignant melanomas [6]. This study was further supported by findings by Vaupel and colleagues that tumour hypoxia acting though direct or indirect mechanism or both may contribute to resistance to radiotherapy, some chemotherapy regimens and chemoradiations [7]. Tumour oxygenation is mainly affected by the rate of blood flow, micro-circulation and haemoglobin concentration; therefore, correcting the Hb level will improve the tumour oxygenation [8]. There is also enough evidence to suggest that, regardLess of the treatment, patients with hypoxic tumours are likely to have less local disease control and fewer cures, compared with patients with better oxygenated tumour of the same size and stage [9].
There are three explanations for the adverse impact of tumour hypoxia on survival. First, hypoxia induces expression of vascular endothelial growth factor (VEGF) which stimulates angiogenesis and increase the potential for tumour growth and metastasis; Second, ionizing radiation results in the formation of free radical within the cells. In the presence of oxygen, the free radicals are fixed and interact with DNA and cell membrane to cause cell death. When cells are hypoxic, the free radicals are not fixed and cell death may not occur; Third, hypoxia may produce a growth advantage for tumour cells that are resistant to apoptosis, with a decrease in potential for cure or control [10]. According to National Cancer Comprehensive Network (NCCN) anaemia is defined as inadequate circulating level of haemoglobin or red blood cells normal for an individual [2]. Anaemia is further classified based on severity by NCCN into mild (10 g/dL), moderate (8.0 - 9.9 g/dL), severe (6.5 - 7.9 g/dL) and life threatening less than (< 6.5 g/dL).
Ludwig et al. examined 9,118 cancer patients using Hb concentration level less than 12 g/dL as the baseline value to study frequency of anaemia in various cancer types. The results of these studies were expressed in percentages: Breast cancer - 26%, Lung cancer - 48%, Colorectal - 33%, Head and Neck - 46%, Gynaecological - 43%, Lymphoma and Myeloma - 47%, Leukaemia - 53%, Urogenital - 43% and others - 37%. [3], Institute of Human Virology of Nigeria (IHVN) analyzed data from [11] Hospital Based Cancer Registry Programme in Nigeria from 2009 – 2010. The study revealed that the commonest five cancers in males and females were as follows: Male – Prostate cancer 29.2%, Colorectal cancers 7%, Lymphomas 6.8%, Liver cancers 4%, Skin cancers 3.8%. In females, the commonest cancers were as follows: Breast cancers 40.4%, cervical cancers 17.3%, ovarian cancers 3.7%, lymphomas 3.1% and skin cancers 2.1% [11]. The conclusion of this study was that Breast and Cervical cancer accounts over 60% of all cancer cases affecting Nigerian women. While in the males, prostate and colorectal cancers are the most common cancers in males aged 45 years and above.
Also, studies done by Ludwig et al. on anaemia prevalence in patient receiving different cancer treatment with anaemia defined as Hb concentration level less than 12 g/dL was quite significant. The results were as follows: Chemotherapy - 75%, combination of Chemotherapy and Radiotherapy - 72%, concomitant Chemotherapy and Radiotherapy - 62%, No treatment -40% and Radiotherapy alone - 38% [3].
Materials and Methods
A prospective study of anaemia in cancer patients undergoing Radiotherapy and Chemotherapy was used in treatment of 201 patients with histopathologically confirmed diagnosis of cancer (solid cancers) that were referred to the Radiation Oncology Unit of National Hospital Abuja. Informed consent was obtained from participants and ethical approval from National Hospital Ethical Board prior to commencement of the study. Patient’s WHO performance status was chosen as 0 and 1. All the enrolled patients had their baseline or pretreatment Hb level measured at first consultation. Those who met the inclusion criteria were followed up in the course of therapy by measuring their on-treatment Hb level once every two (2) weeks. Blood film pictures of the patients were examined during therapy. Patients were subsequently categorized into three arms: Chemotherapy alone, Radiotherapy alone and Chemoradiation therapies.
This on-treatment Hb measurement was terminated after three (3) consecutive determination of Hb concentration level i.e., sixth week. The Radiotherapy machine energy, dosage, field size and number of fractions were recorded in the course of the study. For those undergoing Chemotherapy, regimen, frequency of administration, dosage, and route of administration and also the number of cycles were recorded. Those on Chemoradiation were evaluated for energy, dose, field size, treatment site and Chemotherapy regimen used. All collected data was analyzed using IBM statistical package for social sciences (SPSS) version 20. Continuous variables were summarized using mean and standard deviation (SD). Categorical variables were summarized as proportion and percentages. Comparison of mean Hb level based on sex was made using the student T-test at significant p-value level of ≤ 0.05. Anaemia was classified for this study into: Less than 10 g/dL - Severe anaemia, 10 - 10.9 g/dL - moderate anaemia, 11 – 11.9 g/dL - mild anaemia, 12 g/dL and above - no anaemia.
Results
Table 1 shows demographic characteristics of the studied patients. Majority of patients that had different treatment modes were aged 35 – 44 years; Chemotherapy 36 (36.0), Radiotherapy 19 (30.2) and Chemo-Radiotherapy 11(27.7). Equally most were females Chemotherapy 88 (88.0%), Radiotherapy 58 (92.1) and Chemo-Radiotherapy 27 (71.1).
| Age group | Mode of Treatment | ||
|---|---|---|---|
| Chemotherapy | Radiotherapy | Chemo-Radiotherapy | |
| N = 100 | N = 63 | N = 38 | |
| Number (%) | Number (%) | Number (%) | |
| 25 – 34 | 17 (17.0) | 11(17.5) | 7 (18.4) |
| 35 – 44 | 36(36.0) | 19 (30.2) | 9 (27.7) |
| 45 – 64 | 22 (22.0) | 10 (15.9) | 8 (21.1) |
| 55 – 64 | 21(21.0) | 11 (17.5) | 10 (26.3) |
| 65 – 74 | 3 (3.0) | 8 (12.7) | 3 (7.9) |
| 75+ | 1 (1.0) | 4 (6.3) | 1 (2.6) |
| Sex | |||
| Female | 88(88.0) | 58(92.1) | 27(71.1) |
| Male | 22(22.0) | 5(7.9) | 11(28.9) |
Table 1: Demography of the studied patients.
Table 2 shows WHO performance status of the studied patients. Most patients that were of status 0 had Chemotherapy; males 8, females 40 while patients that were of status 1 majority of males had Chemo-Radiotherapy (6) and females Chemotherapy (48).
| Therapy | WHO performance status | |||
|---|---|---|---|---|
| Status 0 | Status 1 | |||
| Male | Female | Male | Female | |
| Radiotherapy | 3 | 35 | 2 | 23 |
| Chemotherapy | 8 | 40 | 4 | 48 |
| Chemoradiation | 5 | 17 | 6 | 10 |
| Total | 16 | 92 | 12 | 81 |
Table 2: Showing WHO performance status of the studied patients.
Table 3 shows relationship between Haemoglobin by sex with mode of treatment. None of the mode of treatment showed a significant difference between males and females (all p>0.05).
| Sex | Chemotherapy Mean (SD) g/dL |
Radiotherapy Mean (SD) g/dL |
Chemo-Radiotherapy Mean (SD) g/dL |
|---|---|---|---|
| Male | 11.72 (0.88) | 10.82 (0.95) | 12.27 (1.39) |
| Female | 11.65 (1.21) | 12.14 (1.02) | 11.13 (1.14) |
| t | 0.53 | -2.96 | 2.41 |
| P-value | p>0.05 (NS)* | p>0.05 (NS) | p>0.05 (NS) |
| * NS =Not Significant | |||
Table 3: Relationship between Hb by sex with mode of treatment.
Table 4 shows distribution of changes in Blood Film by mode of treatment over 6 weeks of treatment. Majority of patients showed Normocytic Normochromic and no blast cells at weeks 0, 2, 4 and 6 for Chemotherapy, Radiotherapy and Chemo- Radiotherapy.
| Week0 | Week2 | Week4 | Week6 | |
|---|---|---|---|---|
| Haemoglobin ( g/dL) | Mean(SD) | Mean(SD) | Mean(SD) | Mean(SD) |
| Radiotherapy | 13.42(1.20) | 12.42(1.51) | 11.99(1.50) | 11.35(1.32) |
| Chemotherapy | 12.55(0.90) | 12.18(0.93) | 12.02(1.10) | 11.83(1.50) |
| Chemo-radiation | 12.34(0.81) | 11.78(0.90) | 11.31(0.93) | 11.17(0.88) |
| Blood Film Picture | n(%) | n(%) | n(%) | n(%) |
| Chemotherapy | ||||
| Normocytic Normochromic | 73(73.0) | 53(53.0) | 45(45.0) | 28(28.0) |
| Hypochromic | 13(13.0) | 20(20.0) | 33(33.0) | 37(37.0) |
| Macrocytosis | 5(5.0) | 5(5.0) | 1(1.0) | 5(5.0) |
| Microcytosis | 2(2.0) | 1(1.0) | 2(2.0) | 1(1.0) |
| Poikliocytosis | 1(1.0) | - | - | 1(1.0) |
| Anisocytosis | 2(2.0) | 14(14.0) | 7(7.0) | 11(11.0) |
| Elliptocytosis | - | 1(1.0) | - | 2(2.0) |
| Dimorphic | 1(1.0) | 3(3.0) | 5(5.0) | 6(6.0) |
| Target Cells | 3(3.0) | 3(3.0) | 7(7.0) | 9(9.0) |
| Blast cells | - | - | - | - |
| Radiotherapy | ||||
| Normocytic Normochromic | 48(76.2) | 42(66.7) | 36(57.1) | 36(57.1) |
| Hypochromic | 6(9.5) | 11(17.5) | 16(25.4) | 17(27.0) |
| Macrocytosis | 2(3.2) | - | 2(3.2) | - |
| Microcytosis | 2(3.2) | - | - | - |
| Poikliocytosis | 1(1.6) | 2(3.2) | - | - |
| Anisocytosis | 1(1.6) | 2(3.2) | 5(7.9) | 2(3.2) |
| Elliptocytosis | 1(1.6) | 1(1,6) | 1(1.6) | 4(6.4) |
| Dimorphic | 2(3.2) | 5(7.9) | 3(4.8) | 4(6.4) |
| Target Cells | - | - | - | - |
| Blast cells | - | - | - | - |
| Chemo-Radiotherapy | ||||
| Normocytic Normochromic | 28(73.7) | 22(57.9) | 10(26.3) | 10(26.3) |
| Hypochromic | 5(13.2) | 10(26.3) | 23(60.5) | 16(42.1) |
| Macrocytosis | 1(2.6) | 2(5.3) | 1(2.6) | 3(7.9) |
| Microcytosis | 1(2.6) | - | - | 1(2.6) |
| Poikliocytosis | 1(2.6) | - | 1(2.6) | - |
| Anisocytosis | 1(2.6) | 4(10.5) | 2(5.3) | 6(15.8) |
| Elliptocytosis | - | - | - | 1(2.6) |
| Dimorphic | 1(2.5) | - | 1(2.6) | 1(2.6) |
| Target Cells | - | - | - | - |
| Blast cells | - | - | - | - |
Table 4: Distribution of changes in haemoglobin and blood film by mode of treatment over 6 weeks of treatment.
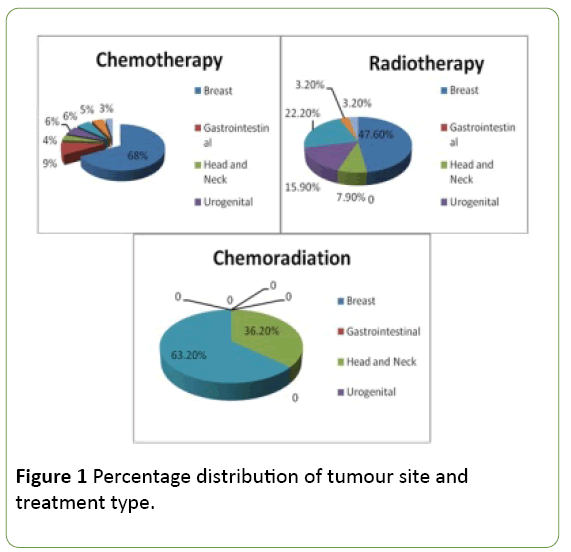
Figure 1 shows percentage distribution of tumour site and treatment type. While higher proportion of patients that received Chemotherapy (68.0%) and Radiotherapy (47.6%) had breast cancer higher proportion that received Chemo- Radiotherapy (63.2%) had gynecological cancer.
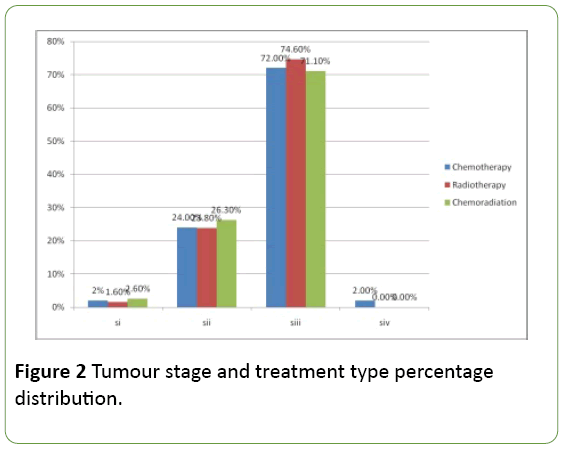
Figure 2 shows tumour stage and treatment type percentage distribution. Most patients were at stage 3 and received similarly chemotherapy, radiotherapy and chemoradiotherapy for stages 1 to 4 while those at stage 4 received only chemotherapy.
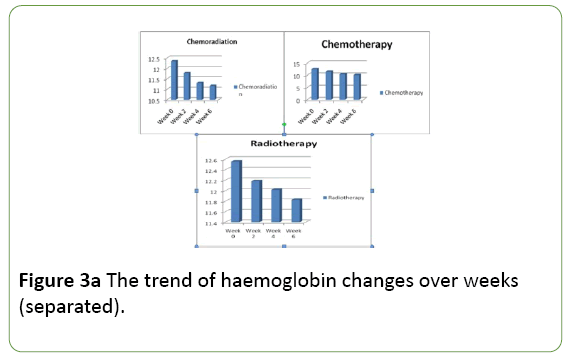
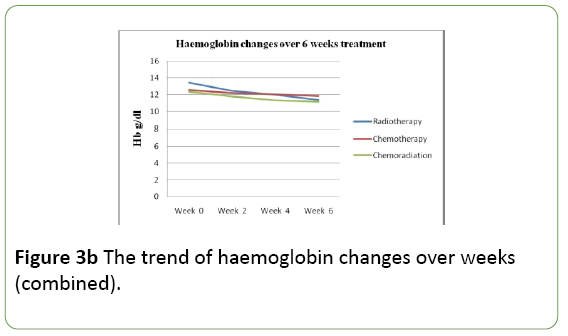
Figures 3a and 3b shows the trend of Haemoglobin changes over weeks. There was gradual but continuous fall in Haemoglobin level for all modes of treatment though it is less marked for Chemotherapy
Discussion
In this study a total of two hundred and one (201) cancer patients undergoing Radiotherapy and Chemotherapy at the National Hospital Abuja were analyzed. Majority of the cancer patients in this study were female making up 86.1% while only 13.9% were male. This finding was in agreement with the studies done by other researchers [3,12]. The sex distribution above was found to be in contrast to many other studies which showed that male cancer patients generally were in higher proportion than female cancer patients [13-17]. This may be due to the differences in population studied or treatment options at the facility. The implication is that it is very challenging bearing in mind the important role women play in family day to day activities. In this study the age range of the cancer patients analyzed was between 25-75years with a median value of 50 years. This report was in contrast to median age of cancer patients evaluated in different studies where cancer cases were found mostly in the middle aged and elderly patients. The median age of cancer patients were found to be above 55 years in a number of studies [3,12,18,19]. This finding shows that working class people are mostly affected and may contribute to high dependence rate with its far reaching burden to the society at large.
In our study, breast was found to be commonest site of tumour site for patients undergoing Chemotherapy and Radiotherapy. This can be partly explained by the fact that most patient studied had cancer of the breast. Equally the single treatment option is the commonest mode of treatment as each has its attendant side effects including Anaemia. This finding was supported by studies done by other researchers [5,7,20-22]. Out of 38 patients on Chemoradiation analyzed, commonest tumour site was gynaecological (63.2%). This study was in agreement with studies done by Morris et al. who studied cancer patients who had Chemoradiation involving gynaecological and head and neck tumours [23]. There was gradual decrease in Hb level over the 6 weeks of treatment for all treatment modes. This gradual decline in Hb level in cancer patients undergoing Chemotherapy in this study was in agreement with the work done by Barrett-Lee et al. [24].They observed that when the patients were analyzed to determine relative risk of anaemia, 62% of patients experienced an Hb decline of 1.5 g/dL within a median of 6.1 to 7.2 weeks and 51% had a Hb decline of 2 g/dL with a median of 7.3 to 8.3 weeks. At the completion of Radiotherapy at week 6, 55.6% of the patients had haemoglobin value at the range of 11-12 g/dL. There was gradual decline in Hb level as the Radiotherapy treatment proceeded from week 0 to week 6. The result of this study was in agreement with work done by Harrison et al. [25] which reported that 41% of patients were anaemic with Hb level less than 12 g/dL before starting Radiotherapy. Out of 38 patients analyzed on Chemoradiation only 4 had Hb level greater than 12 g/dL. This report was in agreement with study done by Mac-Rae et al. [26] following evaluation of 104 cancer patients with stage III non-small cell lung cancer (NSCLC) undergoing ChemoRadiotherapy. The changes in mean Hb over 6 weeks was also in agreement with report by Ludwig et al. [3] which found that cancer patients treated and evaluated after; that anaemia occurred in 50.5% of those who received Chemotherapy, 43.5% of patients who received Chemoradiation and 28.7% in patients who received Radiotherapy.
At the end of therapy 28% of 100 cancer patients on Chemotherapy, 57.1% of 63 patients on Radiotherapy and 26.3% of 38 patients on Chemoradiation therapy respectively had normocytic normochromic blood picture. While 72%, 42.9% and 73.7% were anaemic respectively at the end of therapy. The above observation helped to strengthen our earlier report that Chemotherapy had greatest impact on Hb level during therapy. This assertion was supported by three different studies elsewhere Ludwig et al. Grossi et al. and Jassen et al. which showed that Chemotherapy is a well-known bone marrow depressant and acute cytotoxic agent [3,27,28], To reduce a lot of confounding factors which will likely influence the results of this study, patients that had World Health Organization (WHO), performance status of 0 and 1 were selected. Out of 201 patients studied, 54% (108) had WHO performance status of 0 while 46% (93) had WHO performance status of 1. The correlation between patients’s WHO performance status Hb levels was elucidated by Natacha et al. in their study of 1,403 cancer patients [13]. In their study, there were more patients at enrolment with poor performance status at lower Hb level than at higher Hb levels. WHO score of 2 to 4 were recorded for 65% of patients; with Hb less than 8 to 9.9 g/dL, 22% of those with Hb between 10 – 11.9 g/dL, and 1% of those with Hb greater than 12 g/dL. With this analysis by Natacha et al. it was wise to select patients with good WHO performance status hence the justification for this criteria of choosing patients with WHO performance status of 0 and 1 in this study. Also, Kosmidis et al. observed that at low level of Hb some cancer patients may experience severe anaemia-related symptoms that have a profound effect on their quality of life (QoL), physical and mental functioning and subjective sense of well-being [29]. It was found from the study that the prevalence of anaemia in cancer patients undergoing Radiotherapy and Chemotherapy at National Hospital Abuja was 63% of the study group (ie average of 72%, 42.9%, and 73.7%).
Conclusion and Recommendations
Prevalence of anaemia in the study was high at end of study period. The impact of Chemotherapy on Hb level was more significant than in other treatment arms. The HB level continually decreased in all arms of treatment. This is equally supported by the blood film which showed a marked change in proportion with norrnocytic and normochromic features. Consideration of treatment of mild- to- moderate anaemia will likely become more important as greater emphasis is placed on quality of life (QoL) in the management of cancer patients. We recommend a benchmark of 11 g/dL minimum for any patient being selected for Radiotherapy, Chemotherapy and Chemoradiation in Nigeria as any level lower than this there is high chance of patient having severe anaemia in course of treatment which will have grave consequence on treatment outcome.
Limitations of the study
Paucity of published data in this area in Nigeria was a major challenge, the sample size also might not be adequate for generalization and financial limitation did not allow the expansion of this research to hospitals in poor rural settings in Nigeria.
Acknowledgements
We want to thank National Hospital Abuja, Nigeria for giving us research grant to carry out this study in our centre. We appreciate the effort of Osaretin Shola who typed the manuscript. We extend our appreciation to the following people – Mrs. Aruah Favour, David Aruah, Miss Joy, Prosper, Dr. Ige T, Dr. Adenipekun, Baba Ojebode Jacob, Chief Okoye Nerius and Staff of Radiation Oncology Department, National Hospital Abuja, Nigeria. We equally thank our cancer patients who participated in this study. We are grateful.
References
- Miller CB, Jones RJ, Piantadosi S, Abeloff MD, Spivak JL (1990) Decreased erythropoietin response in patients with the anaemia of cancer N Engl J Med 322: 1689-1692.
- National Comprehensive Cancer Network (NCCN) (2009) Clinical Practice Guideline in Oncology Cancer and Chemotherapy induced anaemia.
- Ludwig H, Belles V, Barrett-lee P,Birgegård G, Bokemeyer C (2004) The European Cancer Anaemia Survey (ECAS) A large multinational prospective survey defining the prevalence, incidence and treatment of anaemia in cancer patients Eur J Cancer 40: 2293-2306.
- Demitri GD (2001) Anaemia and its functional consequences in cancer patient:current challenges in management and prospects for improving therapy. Br J Cancer. 84: 31-37.
- Molls M, Stadler P, Backer A, Feildeman HJ, Dunst J (1998) Mechanism of action, Correlation to low haemoglobin levels. StrahlentherOnkol174: 3-6.
- Nordsmark M, Overgeard M, Overgeard J (1996) Pre-treatment oxygenation predicts radiation response in advanced squanous cell carcinoma of head and neck, RadiotherOncol 41: 31-39.
- Vaupel P, Mayer A (2005) Hypoxia and anaemia: Effect on tumour biology and treatment resistance”. TransfüsClinBiol 12: 5-10.
- Kellerher DK, Mattiensen U, Thewa 0, Vaupel P (1996) Blood flow, oxygenation and bioenergetic status of tumour after erythropoietin treatment in normal and anaemia rats. Cancer Res 56: 4728-4734.
- Hockel M, Schlenger K, Arral B (1996) Association between tumour hypoxia and malignant progression; The clinical evidence in cancer of the uterine cervix. Cancer Res 56: 4509-4515.
- Höckel M, Schlenger K, Aral B, Mitze M, UweSchäffer et al (1996) Association between tumour hypoxia and malignant progression: The clinical evidence in cancer of the uterine cervix. Cancer Research 56: 4509-4515.
- Institute of Human Virology of Nigeria (IHVN) (2012) Cancer Registration in Capacity Development for Research into Aids-Associated Malignancies (CADRE). Department of Virology.
- Santini D, Vincenzi B, Navajas A, Virzi V, Navajas F, et al. (2005) A new dose-intense epoietinalfa regimens effective in anaemia cancer patients receiving chemotherapy: An open-label, non-randomized pilot study. Anticancer Res 25: 669-674.
- Verbeke N, Beguin Y, Wildiers H, Canon JL, Bries G, et al. (2012) High prevalence of anaemia and limited use of therapy in cancer patients: A Belgium Survey (Anaemia day 2008) Support Care Cancer 20: 23-28.
- Laurie SA, Ding K, Whitehead M, Feid R, Murray N, et al. (2007) The impact of anaemia on outcome of Chemoradiation for limited small-cell lung cancer: A combined analysis of studies of the National Cancer Institute of Canada Clinical Trails group. Ann Oncol 18: 1051-1055.
- Pilar M, Samper OTS, Munoz J, Biete A, Ortiz MJ, et al. (2011) PITASOR Epidemiological study: Prevalence, incidence and treatment of anaemia in radiation therapy oncology department in Spain. ClinTranslOncol 13: 322-327.
- Doni L, Penn A, Manzione L, Gebbia V, Mattioli R, et al. (2011) The impact of anaemia on quality of life and hospitalization in elderly cancer patients undergoing Chemotherapy. Crit Rev Oncol Hematol.77: 70-77.
- Vansteenkiste J, Pirker R, Massuti B, Barata F, Font A, et al. (2002) Double blind, placebo- controlled, Randomized phase III trial of Darbepoietinalfa in lung cancer patients. J Natl Cancer Inst 94: 1211-1220.
- Guardiola E, Morchhauser F, Zambrowski JJ, Antonie EC (2007) Management of anaemia in patients with cancer: Results of the FFACT study (French Anaemia Cancer Treatment). Bull Cancer 94: 907-914.
- Seshadri T, Prince HM, Beu DR, Coughlin PB, James PP, et al. (2005) The Australian Cancer Anaemia Survey: A snapshot to anaemia in adult patients with cancer. Med J Aust 182: 453-470.
- Chem AY, Chou R, Shil SJ, Lau D, Gandara D (2004) Enhancement of radiotherapy with DNA Topoisomerase I-Targeted drugs. Crit Rev OncolHaematol 50: 111-119.
- Overgaard M, Nielsen HM, Overgaard J (2007) Is the benefit of post mastectomy irradiation limited to patients without or more positive nodes, as recommended in international consensus reports? A subgroup analysis of the DBCG82b and C randomized trials. RadiotherOncol 82: 247-253.
- Recht A, Edge SB, Solin LJ, Robinson DS, Estabrook A, et al. (2001) Post-mastectomy Radiotherapy: Clinical practice guidelines of the American Society of Clinical Oncology. J Chin Oncol 19: 1539-1569.
- Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, et al. (1999) Pelvic irradiation with concurrent Chemotherapy compared with pelvic and para-gortic radiation for high-risk cervical cancer. N Engl J Med 340: 1137-1143.
- Barrette-Lee, Ludwig H, BirgegardG (2006) Risk of anaemia on patients receiving cycles of Chemotherapy. Oncology 70: 34-48.
- Harrison L, Shasha D, Shiaova L, White C, Ramdeen, et al. (2001) Prevalence of anaemia in cancer patients undergoing radiation therapy. SeminOncol 28: 54-59.
- MacRae R, Shyr Y, Johnson D, Choy H (2002) Declining haemoglobin during chemoRadiotherapy for locally advanced non-small cell lung cancer is significant. RadiotherOncol 64: 37-40.
- Grossi A, Balestri F, Santini S (2007) Darbepoietin alpha in the treatment of cancer Chemotherapy-induced anaemia. Ther Chin Risk Manag 3: 269-275.
- Jessen BA, Lee L, Koudriakova T, Haines M, Lundgren K, et al. (2007) Peripheral white blood cell toxicity induced by broadspectrum cyclic independent kinase inhibitor. J. ApplToxicol 27: 133-142.
- Kosmidis P, Krzakowski M (2005) Anaemia profile in patients with lung cancer. What we have learned from the European Cancer Anaemia Survey (ECAS)? Lung Cancer 50: 401–412.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences