Combined Surgery, Chemotherapy and Radiotherapy of Primary Pulmonary Malignant Fibrous Histiocytoma: A Case Report
Xiaobing Feng, Lele Song, Yuhai Zhang, Shaolin Meng, Xiaojing Wang and Yuemin Li
DOI10.21767/2576-3903.100007
Xiaobing Feng, Lele Song, Yuhai Zhang, Shaolin Meng, Xiaojing Wang and Yuemin Li*
Department of Radiotherapy, The Chinese PLA, 309th Hospital, Beijing, P.R. China
- *Corresponding Author:
- Yuemin Li
Department of Radiotherapy
The Chinese PLA, 309th Hospital
Haidian District, Beijing 100091, P.R. China
Tel: 86-10-66775222
E-mail: liyuemin224@sina.com
Received date: December 20, 2016; Accepted date: December 27, 2017; Published date: January 12, 2017
Citation: Feng X, Song L, Zhang Y, et al. Combined Surgery, Chemotherapy and Radiotherapy of Primary Pulmonary Malignant Fibrous Histiocytoma: A Case Report. J Neoplasm 2017, 1:2. doi: 10.21767/2576-3903.100007
Abstract
Primary pulmonary soft tissue sarcomas are a type of rare malignant tumor that could be misdiagnosed as intimal pulmonary carcinomas or metastasis of other carcinomas. Malignant fibrous histiocytoma (MFH) is one type of the soft tissue sarcoma. The MFH is often seen in deep soft tissue of the extremities, trunk and peritoneum, while primary MFH in lung is rarely seen. Here we report a case of a 46-year-old woman who first presented shoulder pain and a mass lesion occupying almost 1/2 of the left hemi thorax. A malignant pulmonary tumor was considered, and an exploratory thoracotomy was performed. Due to severe adhesion with pulmonary artery, the tumor was not completely removed. Subsequent pathological examination identified the lesion as primary pulmonary malignant fibrous histiocytoma. Combined chemo- and radiotherapy were performed after exploratory surgery and exhibited good therapeutic effects. The patient is on regular follow-up for six years and is currently recovering well with no evidence of relapse. The aim of this case report is to share our experience in treating rare primary pulmonary MFH with combined surgery, chemo- and radiotherapy.
Primary pulmonary soft tissue sarcomas are a type of rare malignant tumor that could be misdiagnosed as intimal pulmonary carcinomas or metastasis of other carcinomas. Malignant fibrous histiocytoma (MFH) is one type of the soft tissue sarcoma. The MFH is often seen in deep soft tissue of the extremities, trunk and peritoneum, while primary MFH in lung is rarely seen. Here we report a case of a 46-year-old woman who first presented shoulder pain and a mass lesion occupying almost 1/2 of the left hemi thorax. A malignant pulmonary tumor was considered, and an exploratory thoracotomy was performed. Due to severe adhesion with pulmonary artery, the tumor was not completely removed. Subsequent pathological examination identified the lesion as primary pulmonary malignant fibrous histiocytoma. Combined chemo- and radiotherapy were performed after exploratory surgery and exhibited good therapeutic effects. The patient is on regular follow-up for six years and is currently recovering well with no evidence of relapse. The aim of this case report is to share our experience in treating rare primary pulmonary MFH with combined surgery, chemo- and radiotherapy.
Keywords
Soft tissue sarcoma; Malignant fibrous histiocytoma; Lung cancer; Chemo-radiotherapy
Introduction
The World Health Organization (WHO) Consensus Committee defined pulmonary sarcomatoid carcinoma as a group of poorly differentiated non–small cell lung carcinomas that contain a component of sarcoma or sarcoma-like (spindle or giant cell or both) differentiation [1]. The report from Salter et al. [2] suggested that the primary pulmonary sarcomas were particularly uncommon, in which MFH accounts for less than 5% of adult sarcomas. MFH often occurs to lower limbs while rarely occurs in the lung. In this report, we treated a 46-yearold female of primary pulmonary malignant fibrous histiocytoma with surgery and combined chemo radiotherapy, and she has now survived without relapse for 6 years.
Case Report
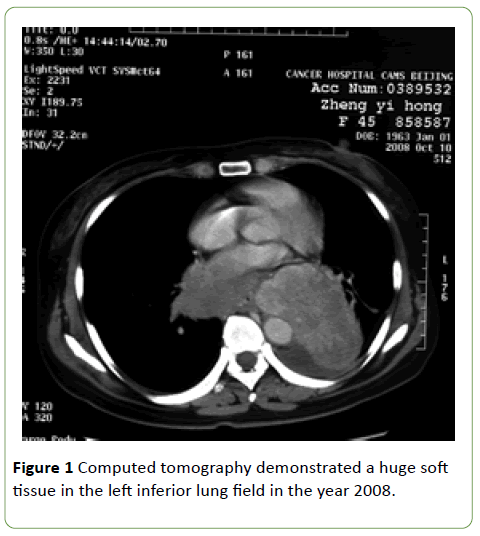
The patient first presented shoulder pain with a huge mass lesion detected by the chest X-ray in the left inferior lung field in another hospital. The computed tomography (CT) scan revealed a large round-shape soft shadow of 6.2 × 9.8 cm with smooth and clear edge (Figure 1).
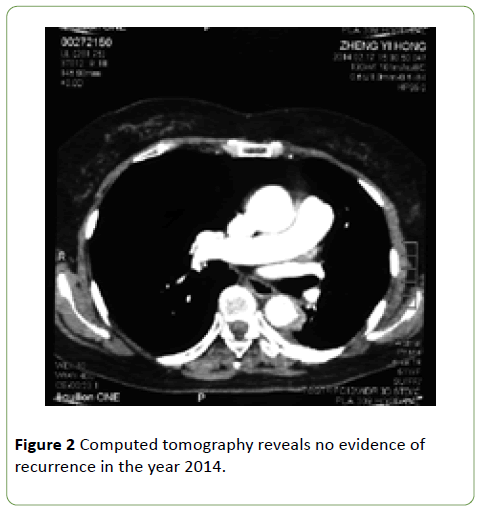
The oesophagus was obviously compressed and the basal segment bronchus of lower lobe of the left lung was also compressed and became narrow. Multiple cysts in the liver were found with CT, while no lesions were found in other organs. The whole body bone scan did not show anything abnormal. Surgery was performed in order to remove the tumor and confirm the diagnosis. Due to the proximity of the tumor to pulmonary artery, the tumor was not completely removed. Immunohistochemistry examination showed positive results for Vimentin, CD68, S100 proteins, and 40% positive for Ki67 Negative results were found for epithelial membrane antigenEMA, AE1/AE3 and CK18. Pathology examination identified a pulmonary soft tissue sarcoma with the subtype of MFH (more specifically, pleomorphic undifferentiated high-grade sarcoma). Based on American Joint Committee on Cancer (AJCC) Staging System for soft tissue sarcoma, the case was categorized as stage III (T2bN0M0G3). Post-operational therapy was performed after the patient recovered from surgery. She received radiation therapy (50Gy fractionated) and two cycles of chemotherapy (Ifosfamide, Dacarbazine, and Cisplatin). CT examination revealed that the radio chemotherapy resulted in complete remission of the tumor. The patient has been examined annually by chest CT and has been in good health condition without relapse (Figure 2).
Discussion and Conclusion
Primary pulmonary soft tissue sarcomas are very rare and preoperative diagnosis of the tumors is very difficult [3,4]. Weiss et al. [5] analyzed 200 cases of MFH and found 68% and 16% of all cases occurs to the limbs and retroperitoneum, respectively. To date, surgery is the most effective treatment of MFH, while there are only a few reports on the effectiveness of chemotherapy or radiotherapy [6,7]. The prognosis of a patient with soft tissue MFH depends greatly on tumor size, location and the adequacy of the initial surgical excision. The 5-year survival rate was 82%, 68% and 51%, respectively for tumors smaller than 5 cm, 5 cm to 10 cm and larger than 10 cm. Furthermore, Pezzi et al. [8] analyzed 227 cases of MFH, and found that the grade and size of the tumor emerge as significant prognostic indicators. Middle-grade and high-grade tumors yield a 5-year survival rate of 80% and 60%, respectively. With the development of surgical and radiotherapy technology, the 5-year survival rate is higher than that of 20 years ago.
In the present case, the tumor was too large to be completely removed and subsequent radiotherapy and chemotherapy were performed to achieve remission. Radiotherapy is a very important part of cancer management, with >50% of all patients undergoing radiation treatment, particularly in the head and neck region. There was no specific data in the utilization of radiation in MHF therapy. Based on some randomized trials in primary soft tissue sarcoma of the extremities, radiotherapy provided an improvement in local tumor control without impact on survival [9]. However, chemotherapy and radiotherapy were not always effective for the treatment of primary pulmonary MFH, since only some cases obtained long-term survival. Surgery is the still most effective treatment for MFH. The patient in this report has been on regular follow-up and has been in good health condition for the past six years. We believe that for some cases, pre-operational radiotherapy, chemo radiotherapy or post-operational chemo- or radiotherapy should be considered. Since there has been no guidance on how preoperational or post-operational chemo- or radiotherapy should be performed, further evidence is still needed to guide the therapy for primary soft tissue sarcoma.
Conflict of Interests
The authors declare that there is no conflict of interests for this study.
References
- Litzky LA (2008) Pulmonary sarcomatoustumors. Arch Pathol Lab Med 132: 1104-1117.
- Salter DM (2006) Pulmonary and thoracic sarcomas. Current Diagnostic Pathology 12: 409-417.
- Tsangaridou I, Papamihalis G, Stathopoulos K, Konstantinopoulos O, Thanos L (2010) Primary malignant fibrous histiocytoma of the lung: a case report. Case Rep Med 1:389-692.
- Aoe K, Hiraki A , Maeda T , Onoda T , Makihata K , et al. (2003) Malignant fibrous histiocytoma of the lung. Anticancer Res 23: 3469-3474.
- Weiss SW, Enzinger FM (1978) Malignant fibrous histiocytoma: An analysis of 200 cases. Cancer 41: 2250-2266.
- Maitani F (2010) A case of juvenile primary pulmonary malignant fibrous histiocytoma. Tokai J ExpClin Med 35: 130-132.
- Yamada N, Minato N, Ikeda K, Shimokawa T, Hisamatsu Y (2003) Surgical treatment of primary pulmonary artery tumor: two cases of malignant fibrous histiocytoma and leiomyosarcoma. Jpn J ThoracCardiovascSurg 51: 557-561.
- Pezzi CM, Rawlings MS Jr, Esgro JJ, Pollock RE, Romsdahl MM (1992) Prognostic factors in 227 patients with malignant fibrous histiocytoma. Cancer 69: 2098-2103.
- Pellizzon AC (2014) Evidence and clinical outcomes of adult soft tissue sarcomas of the extremities treated with adjuvant high-dose-rate brachytherapy - A literature review. J Contemp Brachytherapy 6: 318-322.

Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences